A cleft lip is a split or opening in the upper lip, while a cleft palate is a split or opening in the roof of the mouth. These conditions occur when facial structures don't fully join during fetal development. Cleft lip and cleft palate can occur separately or together.
In the UK, approximately 1 in 700 babies are born with a cleft lip, with or without a cleft palate. This translates to roughly 1,200 babies each year, according to the Cleft Lip and Palate Association.
A cleft palate affects the baby's ability to create the negative pressure needed to suck effectively. This can lead to:
- Poor weight gain
- Fatigue during feeding
- Milk escaping through the nose
- Risk of aspiration
- Frustration for baby and caregiver
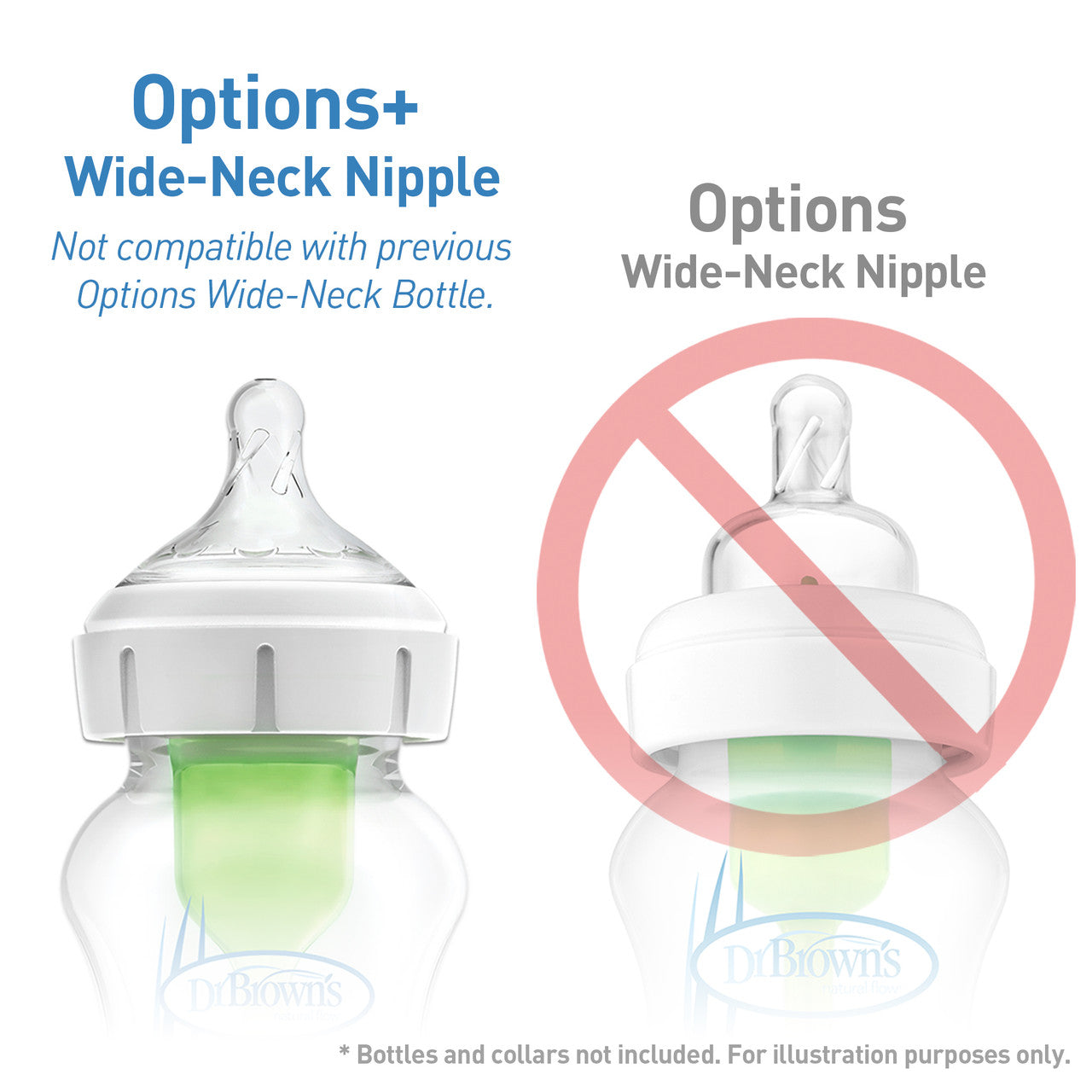
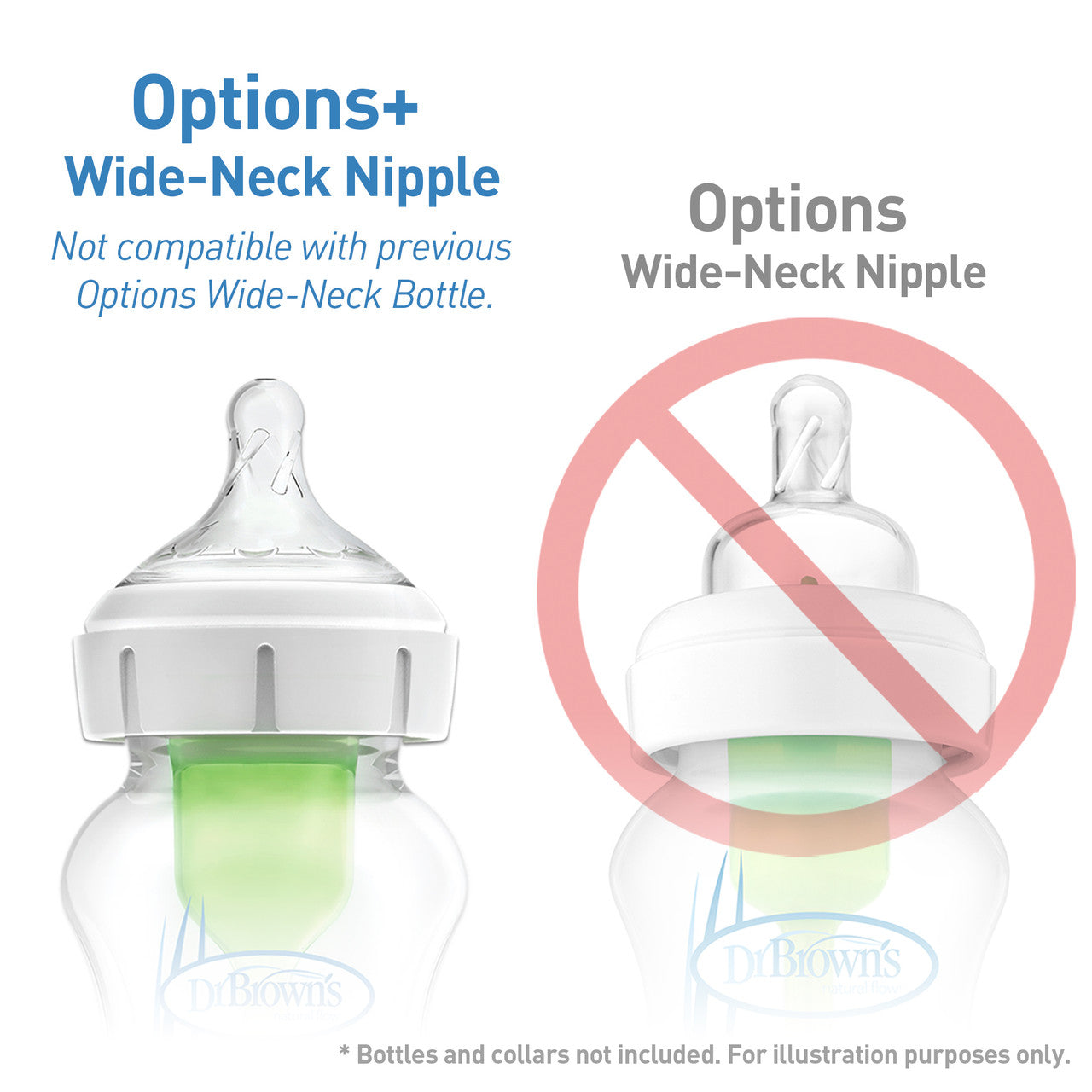
Because babies with cleft palate can’t generate suction, they rely on gravity and gentle compression of the nipple to draw milk. Dr. Brown’s bottles are highly recommended by speech therapists, lactation consultants, and NICU staff.
Pro Tips for Feeding a Baby with Cleft Palate Using Dr. Brown’s
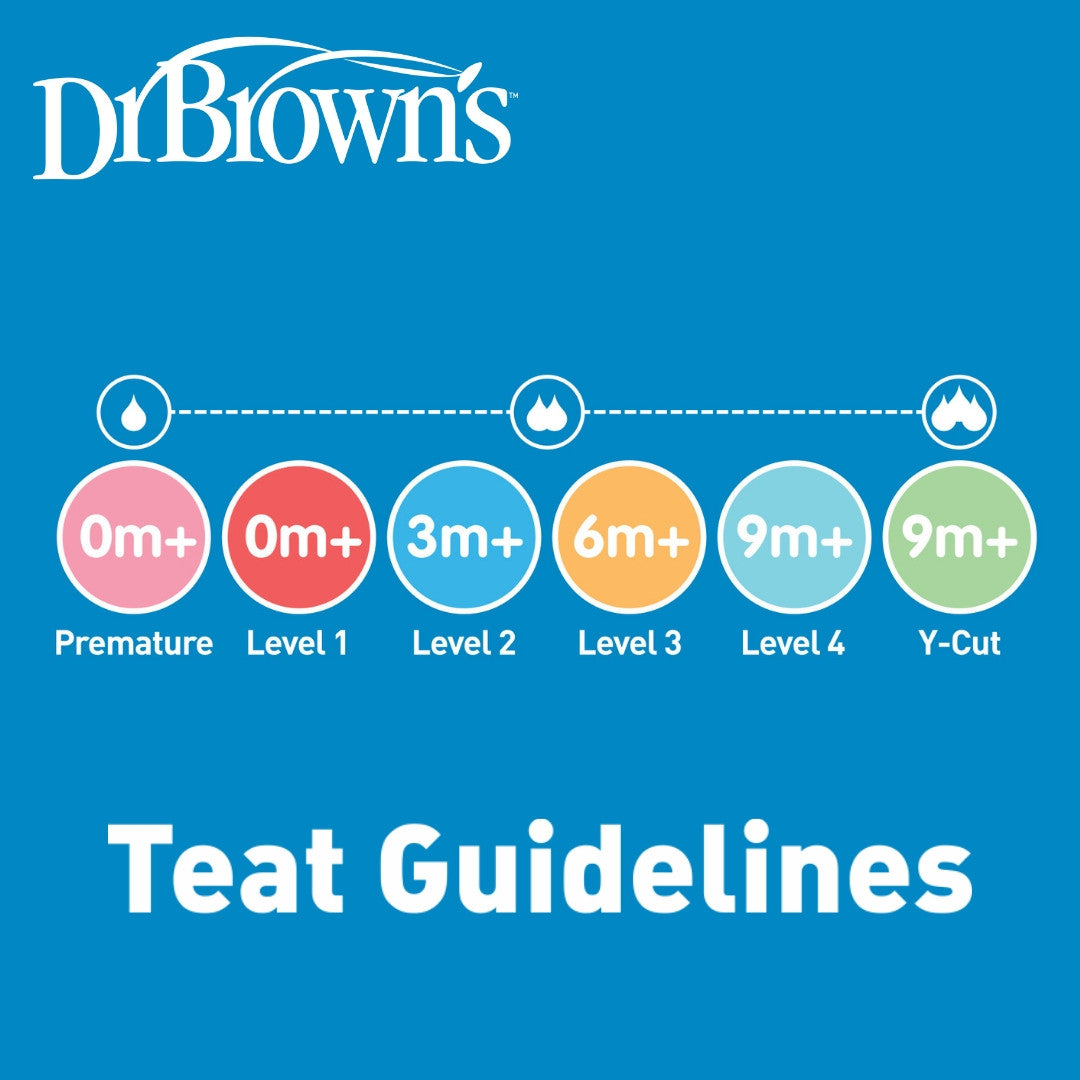
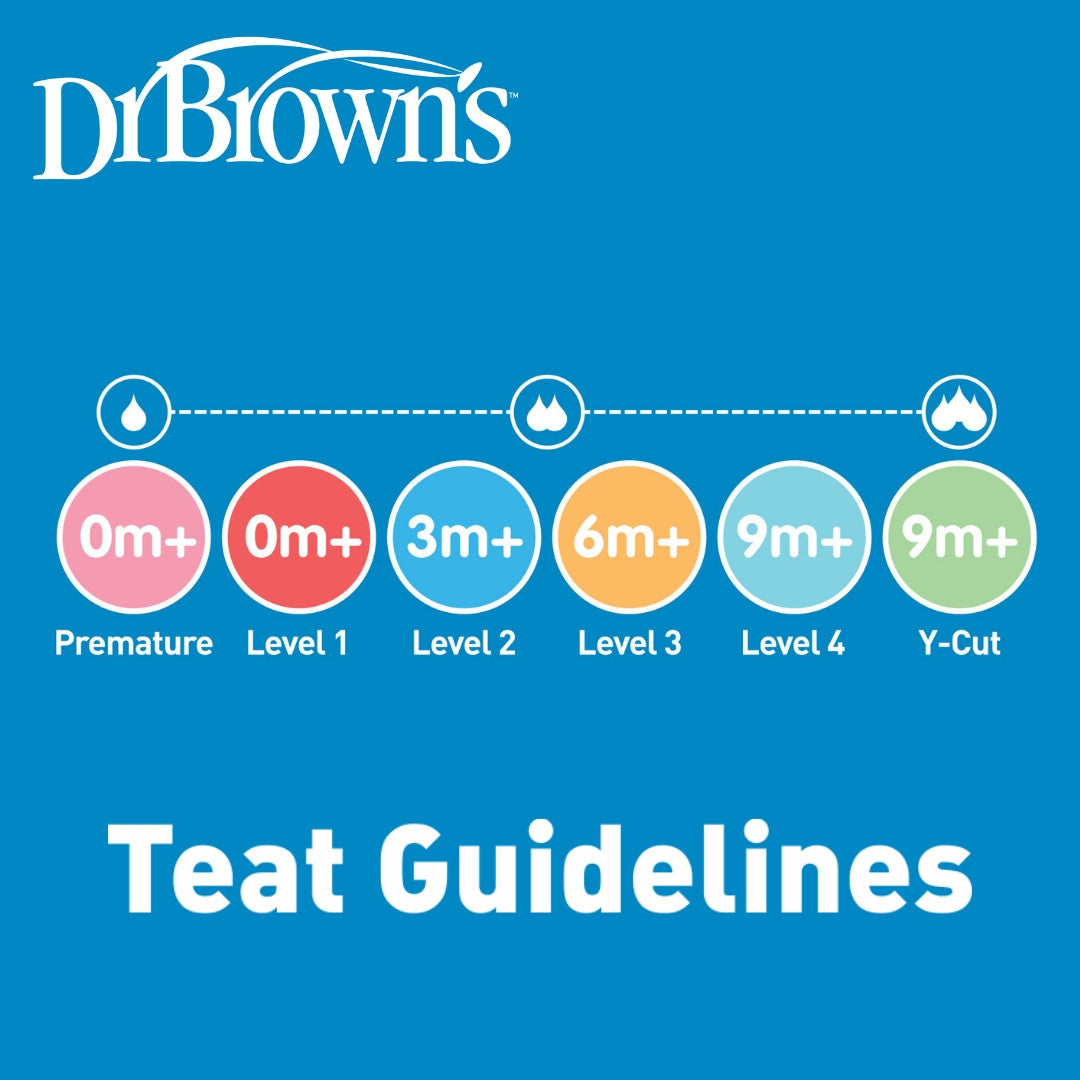
- Use Preemie teats for best control.
- Keep your baby semi-upright to prevent milk from entering the nasal cavity.
- Watch for nasal regurgitation and pause feeding as needed.
- Work with a cleft team (speech-language pathologist, feeding therapist, paediatrician) to tailor your feeding plan.
Can They Still Breastfeed?
Cleft Lip Only? Yes, often.
Many babies with a cleft lip (but an intact palate) can breastfeed well, especially if positioned correctly and with some latch adjustments.
Cleft Palate or Combined Lip + Palate? Not always — but partial or assisted breastfeeding may still be possible.
Most babies with a cleft palate cannot create enough suction to breastfeed effectively. However:
- Some may latch and comfort nurse (even if milk transfer is minimal)
- Others may do "breastfeeding practice" at the breast while getting milk by bottle or supplemental nursing systems
- A few with small or submucous clefts may be able to breastfeed fully
What Are the Alternatives?
If breastfeeding isn’t possible:
- Expressed breast milk can be fed using a our specialised bottles (e.g. Dr. Brown’s with Preemie nipple)
- These bottles allow babies to feed using compression rather than suction
- Parents can still maintain skin-to-skin contact, pumping, and other bonding routines
Tips for Parents
- Consult an International Board Certified Lactation Consultant (IBCLC) experienced with cleft conditions
- Ask for a referral to a cleft team (many hospitals have multidisciplinary teams that include feeding specialists)
- Pumping early and often helps maintain milk supply if direct breastfeeding isn’t working
- Use paced bottle feeding to mimic breastfeeding rhythms
Babies with a cleft palate may not be able to breastfeed in the traditional sense, but they absolutely can:
- Receive breast milk
- Bond at the breast
- Transition to oral feeding after surgery, with support
With the right tools, strategies, and clinical guidance, many parents find a feeding plan that works for both them and their baby — even if it looks a little different than expected.